Dysautonomia POTS
If I've sent you this link, you or someone you love is having some confusing symptoms like spikes in blood pressure, a racing heart rate, heart palpitations, extreme fatigue, dizziness, and fainting. POTS can be difficult to diagnose, but as far as mysterious chronic illnesses go, it's a fairly easy one to manage.
What does POTS stand for and what does it mean?
It's a mouthful. It stands for Postural Orthostatic Tachycardia Syndrome, and even medical professionals sometimes have to ask me how to spell it and what it means.
- Postural refers to the position a person is in (such as sitting or standing).
- Orthostatic refers to a person standing upright.
- Tachycardia (tah-kee-KAR-dee-uh) means fast heart rate.
- Syndrome simply means a specific collection or group of symptoms.
POTS is a type of dysautonomia. Dysautonomia is a disorder of the autonomic nervous system, which means the body struggles to regulate some of its automatic processes, like heart rate, blood pressure, and body temperature.
Usually when a person stands up, the autonomic nervous system tells the blood vessels in the lower body to constrict. This fights the gravitational pull on our blood, preventing it from pooling in the lower extremities. When our blood vessels constrict, it directs blood to the rest of the body to help maintain a consistent and healthy heart rate and blood pressure.
When someone has POTS, the blood vessels in the lower body don't always constrict correctly & doctors don't exactly know why. When those blood vessels fail to constrict, a much lower volume of blood is returned to the brain upon standing. This can cause lightheadedness, dizziness, fatigue, brain fog, and fainting or near-fainting. To combat this, our bodies release emergency stress hormones like epinephrine (adrenaline from the adrenal glands) and norepineprhine (an important hormone in the fight or flight response, released from the nerves themselves) to tighten the blood vessels. These hormones can spike our heart rate, which can cause skipped heart beats, chest pain, and severe shakiness that can look like tremors or a seizure.
POTS presents a little differently for everyone. Some people end up with a drop in blood pressure after standing for a while, while others will experience a spike.
Severity and quality of life
The severity of POTS symptoms run the gamut. Some patients can continue to work, attend school, and participate in social & recreational events with managed symptoms. Others might have symptoms so severe that they require in-home health care and must go on disability. POTS is considered an invisible illness, meaning you can't always tell if someone has it just by looking at them. Some patients aren't allowed to drive, some have driving clearance, but need handicap parking passes.
Due to low blood volume and often extreme fatigue, most POTS patients require more energy to do simple tasks like brushing one's teeth or showering. According to Dysautonomia International, physicians with expertise in treating POTS have compared the functional impairment seen in POTS patients to the impairment seen in chronic obstructive pulmonary disease (COPD) or congestive heart failure. See the study here. The popular spoon theory helps explain this often unseen and misunderstood impact of living with an energy-draining chronic disease. POTS patients often refer to themselves as 'spoonies.'
Is the condition common?
I'd never heard of it until I was (finally) diagnosed, but Dysautonomia International estimates that POTS impacts somewhere between 1 and 3 million Americans, plus millions more across the globe. POTS primarily affects women, but men can also develop the condition. POTS can affect adolescents (symptoms often present during puberty), but presentation in children is uncommon.
POTS sometimes seems to begin after a viral illness or after someone has had surgery or a massive shock like surviving a car accident or witnessing a traumatic event. POTS can run in families but so far, no gene has been isolated or identified. According to Hopkins Medicine, research has shown an overlap between POTS, joint hypermobility, and mast cell disorders, some of which have a genetic origin. If you have hypermobility symptoms, you may want to explore this connection further.
Is there a list of symptoms?
The standard diagnostic criteria is simply an abnormal heart rate upon standing. Patients can experience a drop in blood pressure upon standing or an increase. Most POTS patients have an abnormally low blood volume (hypovolemia) and blood tests can show high levels of epinephrine and norepineprhine if a medical provider takes the blood sample under the correct conditions. Many POTS patients experience the following:
- Severe or long-lasting fatigue
- Headaches including migraines and/or problems with eyesight like blurred vision
- Lightheadedness and dizziness
- Heart palpitations or forceful heartbeats (heart pounding or skipping a beat)
- Chest pain and a shortness of breath
- Exercise intolerance or POTS symptoms becoming worse after increased activity
- Brain fog / diminished concentration / diminished working memory
- Tremulousness, shaking, seizing
- Syncope or near-syncope (fainting or near-fainting)
- Difficulty maintaining body temperature, coldness in the extremities
- A pale face and purple discoloration in hands and feet (harder to see if you have brown or black skin)
- Nausea and vomiting or other issues with your stomach and digestion
- Sleeping poorly or developing insomnia
- Excessive sweating
- A feeling of 'zinginess' or 'buzzing' inside the body when a fainting or dizzy spell is coming on.
- More symptoms here. (Please be careful with the dietary recommendations in that list. Slipping into orthorexia or other eating disorders while trying to find a food-based 'cure' for a chronic disease is a real risk.)
Some things can make POTS symptoms worse:
- Heat (hot day, warm bath or shower, hot tub use)
- Standing or walking for extended periods
- Not drinking enough / failing to keep salt intake high
- Sickness & infection
- Stress and anxiety
- Menstrual cycles
- Migraines
- Migraine triggers such as bright light, flashing lights, or fluorescent lights
How is it diagnosed?
It can be really difficult to get a diagnosis. POTS isn't completely understood by doctors or researchers and symptoms can present so differently patient to patient. Your doctor may run blood and urine tests, run an EKG/ECG, or order a 24 hour (or longer) heart monitor.
The tilt-table test is considered one of the most definitive ways to get a POTS diagnosis. Secured to a special table, the patient's blood pressure, heart rate, and blood oxygens are measured. The table is then raised to an upright position and the same vitals are measured. If, after the position change, the patient's heart rate changed abnormally, their symptoms worsened, or if they developed orthostatic hypotension during the first three minutes of testing, the test result is considered positive for POTS (a diagnosis takes into account a 3 months+ history of other symptoms such as lightheadedness, fainting, or excessive fatigue).
A simpler test may be performed without a tilt table. A practitioner may simply measure blood pressure and heart rate while the patient is lying down, then measure again after the patient stands. If, within ten minutes of standing, the heart rate rises at least 30 beats per minute while the blood pressure remains stable (systolic bp drops no more than 20 mm Hg), the patient is considered positive for POTS (again, taking into account the patient's history of other symptoms). Note: Everyone is a little different, so if you're having a lot of symptoms but your blood pressure isn't 'performing' while at the doctor, see my recommendations in the next paragraph.
If you suspect you might have POTS and are having a difficult time getting your primary care physician or general practitioner to listen to you, get a home blood pressure monitor. A wrist cuff (affiliate link; also available in most drug stores) works well. Keep a record of your resting vs standing blood pressures as well as any readings while you are having active symptoms. An appointment with a cardiologist and a three-month history (with these readings) will go a long way in helping you get a diagnosis or rule out POTS in favor of something else.
Treatment
As with many of these frustrating, lesser-known conditions, there is no cure. However, the condition can be managed at a tolerable level with simple changes and an awareness of one's limitations.
- Fluids, fluids, fluids. Drink at least 48-60oz (2-2.5 liters) a day.
- Increase intake of salt! (This one really broke my FIL's brain as he had recently been told to reduce his sodium intake.) POTS patients NEED more salt. Add it to every meal, keep salt tablets in your car, purse, or gym bag, and drink a dissolved teaspoon in warm water if you're in an active POTS flare (fainting, tremoring, shaking). I like Real Salt (affiliate link), it just tastes better, and they have cute little containers you can keep in your purse or car.
- Avoid alcohol - it really likes to aggravate POTS symptoms because it directs your blood flow to your skin (that ruddy beer drinking glow). Alcohol can also make you pee more which decreases your fluid levels.
- Caffeine sometimes helps POTS patients as it helps constrict blood vessels, but it can aggravate symptoms in others.
- Up your exercise routine - Such a frustrating recommendation when you're fainting in grocery stores, but if you start slowly (with a physical therapist if needed), you can help improve blood circulation and increase blood volume. Gentle yoga is a great option. I like Yoga with Adriene on Youtube. For severe cases where patients can't even sit up, exercises can be started in a supine position; also, try aquatic therapy! It reduces the gravitational pull AND creates pressure around the body like a full-body compression sock. People were always concerned I'd faint in the water while lap swimming, but a) I get a lot of warning if an episode is coming on and b) the water pressure stabilized my blood pressure so I never had an episode in the water.
Practical suggestions & coping mechanisms:
- Compression socks, leggings, and even corsets can give those struggling blood vessels a helping hand. Discuss which types might be best for you with your doctor. Long shopping trips or drives can be saved with a good pair of compression garments.
- For some, raising the head of your bed helps POTS patients sleep a little better
- Explore different postures, desks, footstools, chair heights, recliners, and ball-chairs to help manage POTS in an office or school setting. For example, reclining and using a lap desk, lowering your chair so your legs can stretch out, or putting your legs up on another chair or footstool can all help reduce symptoms.
- Somewhat ironically, sitting too long can increase my POTS symptoms. Intermittently raising my desk to standing height (I purchased this adjustable standing desk on Amazon for my home office) and rocking on a balance board or inflatable stability disk (both affiliate links) keeps my blood flowing better so my heart rate stays stable. I set a timer so I'm standing throughout the day. I've also heard good things about an under-desk treadmill.
- Consider filing for disability. If your POTS symptoms are severe and you can't work, filing for disability (US link) can bring some peace of mind. Filing for disability can be a bear with a lot of hoops to jump through, so if you think this might help, start now.
- A handicap parking pass can be such a lifesaver! You'll need a doctor's approval and a visit to the DMV. In some states, a parking pass comes with additional stickers you can put on your existing license plates, or you can get new license plates with the handicap insignia printed right on it. If you don't look ill, be prepared for snarky comments and rude stares. You might want to add an explanatory bumper sticker. Etsy has a lot of good options.
- Use the motorized carts in grocery stores, amusement parks, shopping malls, and libraries. Note: not all shops have them (I still can't believe Ikea doesn't) and sometimes they are annoyingly low on batteries. Again, an enamel pin or badge, t-shirt, or even an explanatory pamphlet or card can help stop the rude looks you'll get for using a cart if you don't look sick or disabled.
- Add a shower chair to your shower or bath. Bathing yourself can be so exhausting when in a full POTS flare.
- Know your warning signs and lay down when they start. My fainting spells start with muscle jerks that look a bit like Parkinson's tremors. I also get a zingy or buzzy feeling inside and my vision might go a little blurry. If these symptoms start I try to get to a spot where I can lie down immediately. If I can, I will also consume a salt tablet or ask someone to bring me some salt dissolved in water. I have had to lie down in an aisle at Walmart and a Smith's grocery store. Not fun, but better than passing out and hitting my head.
- If you can't lie down and have to remain standing, try crossing your legs with one in front of the other, or shifting your weight from leg to leg. If you're bendy or like yoga, try the tree pose, alternating legs. You can also try rocking back and forth on the balls of your feet, rocking up and down on your toes, clenching your ab muscles and buttocks, and clenching and unclenching your fists.
- Don't be afraid to tell someone next to you on the bus or in line that you might collapse. I have often been held by a stranger while my body restarts. Stickman Communications makes cute POTS explanation cards you can keep on your keychain or quickly hand to someone if you need to lie down in public or are about to slump over or collapse.
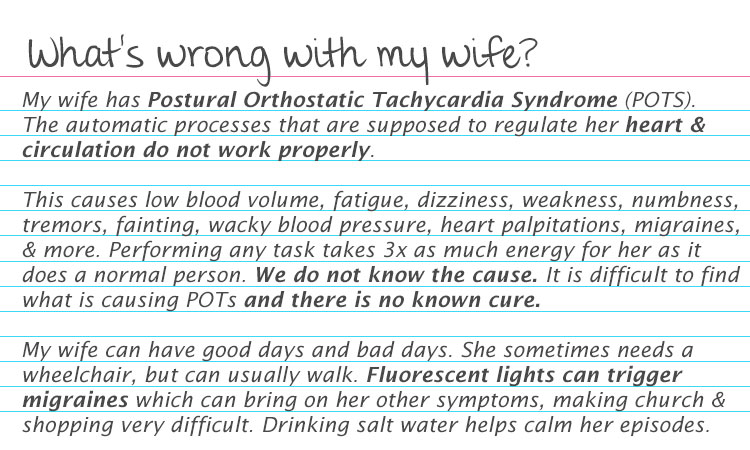
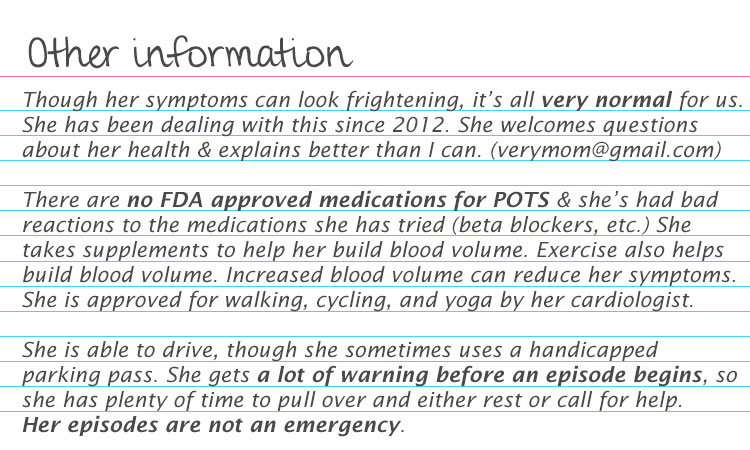
- You can also make your own cards. My husband really struggled to explain what was wrong with me if I passed out or had to lie down while we were in public (everyone wants to call 911!). I made these years ago (printed front & back on one 3x5 card). He kept one in his wallet and just handed it to curious/concerned passerby:
- See a full list of recommendations (treatment and lifestyle) at Dysautonomia International, complete with sources.
Feel free to right-click and save the cards to your desktop if you think they might be useful.
What about medications?
There is no magic pill for POTS, though medication can help improve a patient's quality of life. It can take a lot of trial and error to find the right combo.
Talk to your doctor about medications that might help improve blood volume, help your kidneys retain sodium, or something to help improve the constriction of your blood vessels. Beta blockers are often prescribed to help reduce the heart rate or block that surge of adrenaline that occurs when your autonomic nervous system can't do its job properly. Some serotonin reuptake inhibitors (SSRIs) have been found to be helpful.
Can POTS go into remission?
Yes! Just as suddenly as they appear, POTS symptoms can vanish into the night. They may disappear forever or come back unexpectedly. Sometimes only the major symptoms (fainting, heart palpitations) will disappear, while the extreme fatigue and need to hydrate constantly remain.
After suffering from pretty extreme symptoms for a number of years, most of my POTS symptoms disappeared. I remained easily fatigued, but had a nice long five year break before more symptoms returned.
My story
It was my oldest son's 11th birthday in October of 2012. I collapsed quite suddenly, experiencing near-syncope (I'm not sure I ever passed out completely; it always seemed like I could hear what was going on around me). Everyone (extended family members were in town for the party) assumed I was having a hypoglycemic episode and rushed to bring me orange juice, peanut butter, and string cheese.
It didn't feel like a low blood sugar thing. I'd experienced fainting or blackouts from low blood sugar since childhood and would often get the 'shakes' (dizzy, lightheadedness, hands shaking, sweaty) if I hadn't eaten enough. This felt very different. At the time, the only way I could describe it was as though I had a toilet flush on my forehead; someone had pressed it and all my energy just whooshed right out of my toes, making me feel so weak I couldn't hold myself up.
The day it all started, I had something like 40 near-syncope or full syncope episodes. I don't remember if I started shaking/tremoring right away or if I felt like I was full of bees. I can only remember everyone freaking out and someone calling my neighbor while we waited for my husband, Eric to get home. Eric and my neighbor carried me out to the car together -- it wasn't easy. Without any strength, I couldn't support my own head or limbs. I'm tall and gangly, so it was a trick getting me into the car.

The hospital
Friends met us at the hospital. It was a long wait on a gurney where I felt like I was repeatedly going in and out of consciousness. This part is unusual for POTS: It didn't seem to matter if I was standing, sitting, or lying down, I would still experience fainting or near-fainting. Eventually I got through triage and ended up getting admitted.
I think I stayed in the hospital for around three days while I underwent a battery of tests (including a psyche evaluation to make sure I wasn't having a mental break--I wasn't). It seemed like they drew buckets of blood. The test that stands out most vividly is the Electroencephalogram (EEG) to test for epilepsy (so I must have started tremoring right from the start; I just don't remember). I had a regular EKG, then an echocardiogram, then an echocardiogram with bubble study. Later, I also had another bubble test with doppler to see if the injected bubbles were crossing through to my brain (an indicator for stroke risk), they were.
They did find a fairly large hole in my heart, an 11mm PFO (patent foramen ovale). PFOs are normal in about a quarter of the world's population and most grow old without ever knowing they are there. They can sometimes lead to strokes, so I had an MRI, but no evidence of an even minor TIA (transient ischemic attack) showed up. Still, certain this hole was what was causing my fainting episodes, we traveled to Salt Lake City where a cardiologist closed it with a Gore Helix device.
The FDA no longer (I'm unclear as to whether or not they ever did) approves closing PFOs without a history of strokes, but the PFO closure helped me feel so much better. I stopped passing out for two whole years and the severity of my migraines reduced significantly. I suppose it could have been a placebo effect, or simply feeling better with more oxygen returned to my cells & brain. Interestingly, as of 2023 (over 10 years later), my migraines have remained mild. I used to get them on a debilitating level a couple times of month. I might only get two a year that are bad enough to blind me (I get migraines with aura).
Relapse
My POTs symptoms came back about two years later during a period of high stress. We had sold our family business and I was the primary breadwinner while my husband took care of our four children. I ran a web design company and my biggest client was controlling, manipulative, and borderline abusive. I felt horrifically trapped while this client took advantage of me, grossly underpaid me, and attempted to commit fraud by withholding pay in order to force me into signing a contract without legal advise. I cried every night for months while my husband begged me to fire the client. But our financial situation was precarious after a failed investment in a family company; we were on the brink of bankruptcy (narrowly avoided) and trying to sell our house.
I did eventually fire the client and worked hard over the next several years to improve our stressful circumstances, but had to manage POTS symptoms along with a resurgence of severe chronic hives for the next three years. It was somewhere in here, maybe 2016 or so? that I finally had the tilt table test and got my POTS diagnosis.
POTS symptoms abruptly disappeared again one day in August, 2017. As of February 2023, I've only had a few severe fainting episodes return since (knock on all the wood things). Everyone in my life expected them to return in full after my sweet husband died suddenly in November 2020. 💔 But they didn't. I wonder if shock held me together for a while. My most recent bad episode was at the funeral of a beloved uncle in December, 2022. It just goes to show even clear triggers don't always behave like you might expect them to (I've had them start while relaxing in bed watching a favorite movie!).
My symptoms and management tactics
Chronic symptoms that never seem to go away include: Stupid levels of fatigue, needing more sleep than most / bouts of insomnia, trouble maintaining body temperature (I am almost always cold), and the way normal activities (showering, getting ready, cooking dinner) seem to take 3-6x the amount of energy a normal person might expend.
Acute symptoms that come on during what I call an 'episode' or 'flare' include: Headaches, blurred vision, a buzzy or 'zingy' feeling inside, jerky body tremors or seizing, a huge spike in fatigue (I am so wrung out after an episode), heart palpitations (not always), chest pain (not always), fainting or near-fainting (can't move or see but I can still hear), a loss of body strength (collapsing or slumping over, even if I remain conscious).
Symptoms that were worse upon onset but aren't so bad anymore: Exercise intolerance was awful at first. I used gentle yoga to work my way up to more activity and worked out more during remission periods. I'm never going to be a hardcore gym rat or climb mountains, but I can follow a workout program now and stay fairly consistent. Reddish/purplish discoloration in my legs can still occur, but isn't as dramatic as it used to be.
My early warning signs & how my episodes play out:
Usually my first sign that an episode is coming on is a zingy or buzzy feeling inside, but sometimes an involuntary tremor comes first (looks like a big muscle jerk). These happen with enough warning that if I'm driving I can pull over and recline my chair to rest. Once the tremors kick in in earnest, I will feel a wave of utter fatigue and then all my energy just seems to drain out of my body and I collapse/slump over or faint.
I am never passed out for long, not even for a full minute I don't think (though they might have been longer in the beginning--now they are only seconds). I can continue jerking/tremoring and intermittently fainting for about an hour to an hour and a half (sometimes a lot longer, but that's my average). If I can lay down, rest, and get some salt water in me, I'll start to stabilize and feel like I can sit up and move normally pretty soon, though I remain tired and can feel utterly wrung out for a while afterward. If I'm home or somewhere comfortable, it's best to just call the day a wash and get in bed to rest. I can be quite headachy after an episode and my body can hurt from the tremoring.
Note! My POTS is somewhat unusual as I don't necessarily have symptoms start because I have moved from a sitting to standing position. Though I did pass the tilt table test with flying colors (my heart rate and blood pressure behave abnormally with position changes). I can be seated pretty comfortably or even lying in bed and those stupid tremors will hit.
Things that can (not always!) bring on symptoms or make them worse:
- Fluorescent lights, bright sunlight, or even the glare from white snow on an overcast day. Forgetting my sunglasses is the worst.
- Standing or walking for extended periods. But sitting for extended periods can bring on symptoms too.
- My menstrual cycle (even after a uterine ablation in 2010), particularly in the cramps/sore breasts stage.
- Stress and anxiety.
- Dehydration, low electrolytes/salts.
- Exhaustion, lack of sleep, insomnia.
- Headache or migraine.
- Mysteriously, nothing at all!
Medications / supplements / practical life changes
The only prescription medication I tried was a beta blocker, but I didn't like how it made me feel. We're not supposed to use the word 'crazy' anymore, but that's how it made me feel--I wanted to unzip my skin suit and hang it on a nail. Not normal, so my doctor weaned me off of it.
Taking iron to help build up my blood volume has been a constant in my life (I was diagnosed with anemia long before I was diagnosed with POTS). I also take magnesium, potassium, and calcium (calcium has to be taken separately from the iron), to help keep those body salts up. I keep Real Salt (affiliate link) on hand (tastes better than regular) for active symptoms and drink a teaspoon dissolved in about 16 ounces of water. For me personally, I see a strong correlation in shortening an episode by drinking salt water.
I still wear compression leggings or compression stockings on the regular. I'm tall with a 36" inseam and finding knee-high compression socks for women proved impossible. I switched to buying men's and was happy to finally have some that went all the way to my knee instead of attempting to cut my calf in half. They help a lot if I need to run a lot of errands, but also help while I'm seated at my desk for long hours.
During active flares / bad symptoms, I sometimes require a wheelchair, handicap parking pass, shower chair, and use the motorized carts at grocery stores. I'm pretty terrified of an active, long-term flare coming back after losing my husband. 💔 He helped transport me from place to place and pushed my wheelchair around.
Helpful resources (some previously linked)
- Invisible Disabilities
- Dysautonomia International's POTS page
- Hopkins Medicine POTS write up
- Cute POTS explanation cards
- POTS explained for kids
- POTS article at Harvard Health
- POTS support group on Facebook - There are lots, research which one you like best, it's always nice to have an understanding community. Check your local hospital or doctor's offices for information on local support groups as well.
- Easy yoga for POTS
- Here is some information on genetic testing for possible hypermobility/mast cell links to POTS - I don't know much about this; there might be newer articles out there if you want to explore further.
- An (old) article about the mast cell activation syndrome (MCAS) and POTS.
If you read the whole thing, congratulations! And my condolences. POTS is very annoying and I am not best pleased when symptoms return or worsen, but between chronic hives and POTS, I'd choose POTS; it's far more manageable.
If you have any questions, feel free to contact me. It's the name of this domain (one word) at the mail service google provides. Let me know if you find any typos or mistakes, or just have something to add. Please note, I am not a fan of MLMs or any other diet or predatory snake-oil cures that promise the moon to vulnerable sufferers of chronic, frustrating diseases (see my hive page for more of a full-bodied rant on these subjects). xx
Copyright © 2004-, Very Mom. All rights reserved.